From Clinics to Community: Exploring the Spectrum of Psychedelic-Assisted Psychotherapy in Australia
Associate Professor Petra Skeffington and Dr Stephen Bright
In 2022, Dr Stephen Bright shared the story of the first person in Australia to legally receive MDMA-assisted psychotherapy for PTSD as part of a clinical trial funded through a small university grant and community donations from PRISM Ltd. Since then, we have provided further MDMA-assisted psychotherapy, in addition to psilocybin-assisted psychotherapy in clinical trials in Perth. Meanwhile, the TGA approved the use of MDMA and psilocybin by authorised prescribers. Demand for psychedelic-assisted psychotherapy (PAP) has never been greater and people are not just accessing these treatments via clinical trials and authorised prescribers.
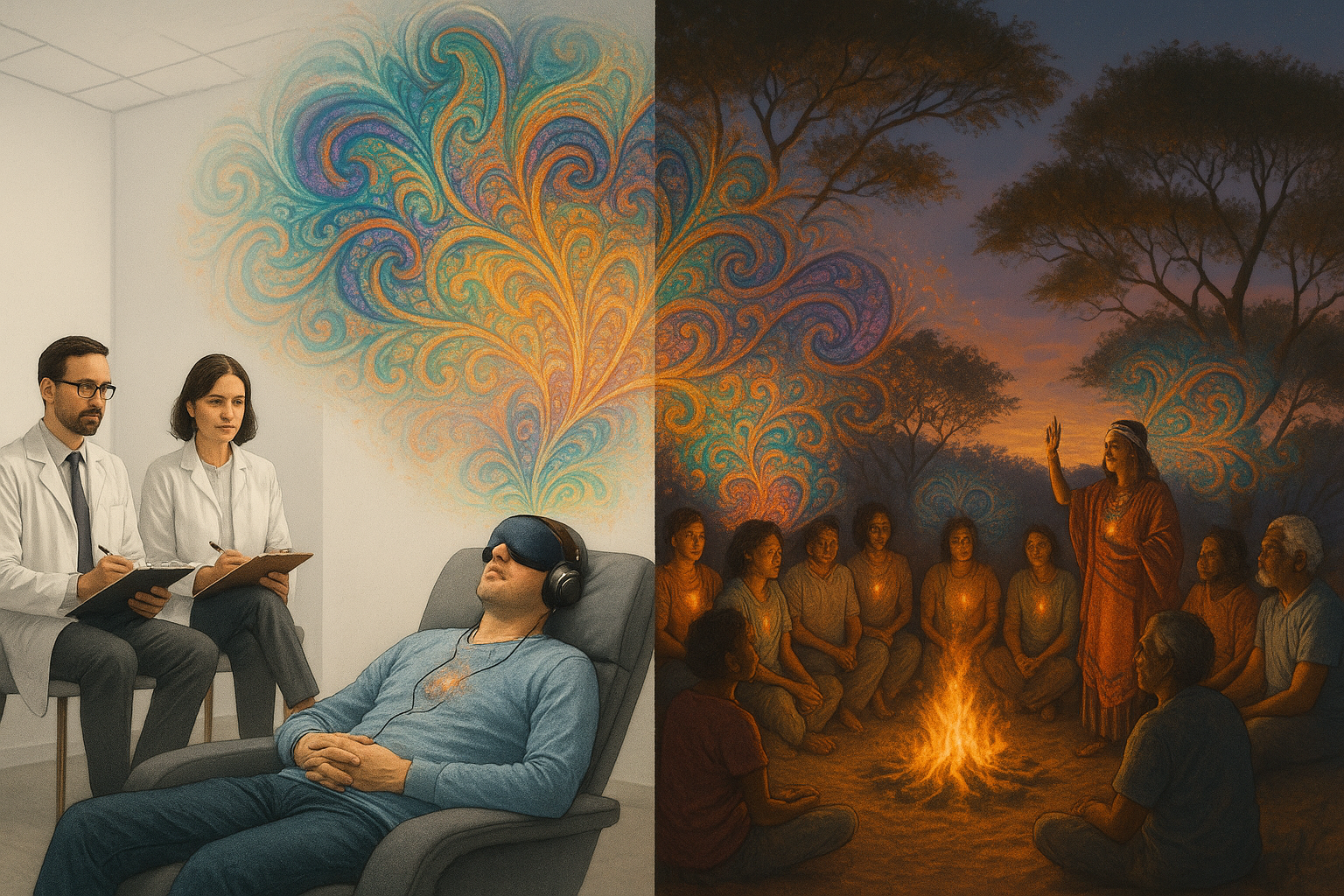
This presentation will explore what we have learned through the lived experiences of individuals undergoing PAP about the suitability of these treatments in a range of different clinical and non-clinical settings. Our aim is not to advocate for one approach over the other, but to clarify the different roles that these therapies can play in healing, depending on the individual and their circumstances. Clinical trials offer safety, oversight, and thorough screening — crucial features for individuals with complex or treatment-resistant mental health conditions. However, these same features can limit accessibility, spontaneity, and personal agency. Underground or community-based approaches, in contrast, can be more adaptive and culturally diverse — but often lack adequate safeguards and integration support. Private (Authorised Prescriber) treatments appear to land somewhere in between.
We will reflect on our experience as psychologists working with both MDMA and psilocybin, focusing on how the "container" — the set and setting, the therapeutic frame, and the intention-holding — plays a central role in shaping the depth and meaning of the psychedelic experience. Without thoughtful integration, the transformative potential of a psychedelic experience may not be fully realised.
Our presentation will include clinical insights from our MDMA and psilocybin trials, including how participants responded to the structure of preparation and integration sessions. We will also reflect on our observations of community-based psychedelic use — informed by dialogue with participants, underground facilitators, and our own broader engagement with the psychedelic community.
At a time when Australia is pioneering the medical use of MDMA and psilocybin, we are also mindful of the deep contribution of those outside the formal system — facilitators, sitters, and elders who have kept the psychedelic healing tradition alive. Both streams, clinical and underground, have much to learn from one another. We look forward to exploring this dialogue.


Associate Professor Petra Skeffington is a Clinical Psychologist in Private Practice, and an academic at Murdoch University in Perth. Her research and clinical expertise centres on psychological trauma and recovery, including resilience to trauma, prevention of post-trauma pathologies, and innovative approaches to treating psychological trauma.